What is Anal Abscess?
Anal abscess occurs as a result of accumulation of pus due to anal gland infection. Anal abscess generally originates from infection of anal glands, and progresses around. Primary function of these glands is to secrete mucus to ease defecation. It is an inflammatory disease requiring immediate surgical drainage. It may occur in any age group, and is more common between the ages of 30-40. Males are more prone to disease than women. It often develops in spring and summer when stool is softer. Runny stool clogs secretion pores of the glands and triggers the disease.
The most common symptoms are pain, irritation, swelling and increased temperature in ano-rectal area. Additionally, symptoms such as anxiety, fever, tremor and sweating may be present. In more severe cases, patients have difficulty in sitting.
The most recognized theory for anal abscess formation is clogging in anal glandular structure, and outspreading of infection originating here to peripheral tissues.
Previous anal abscess history, surgical interventions in the anal area, anal area traumas, anal fissure and fistula presence triggers anal abscess development.
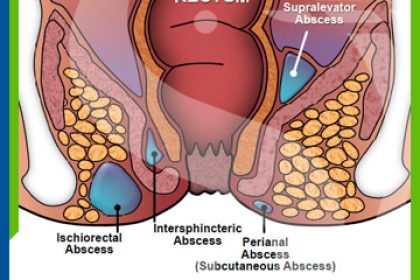
Anal abscesses are analyzed in 4 main groups by their locations. Perianal, intersphincteric, ischiorectal and supralevator.
It is important to suspect the disease for correct diagnosis. Diagnosis can be immediately made by examination in most cases. Ultrasound, MR can be requested if in doubt.
Anal abscess is treated surgically and surgical drainage must be performed under anesthesia. Drainage will be extremely painful without anesthesia.
Antibiotic treatment and patient follow-up is required after intervention.
Patients should be warned against the risk of repeated abscess and fistula development.
Symptoms of Anal Abscess
It begins with pain in anus area during defecation, followed by symptoms such as redness, swelling and increased temperature. Patients also complain about fever, sweating, lethargy and discharge from anus.
Why does Anal Abscess occur?
Previous anal abscess history, surgical interventions in the anal area, anal area traumas, anal fissure/fistula presence are among risk factors for anal abscess development. Sometimes it may occur after extended diarrhea.
Excessive alcohol consumption and obesity are also other the risk factors. Chronic anal fissure can also be reason for anal abscess.
How does Anal Abscess spread?
Due to the pressure exerted by increased amount of pus, intersphincteric abscess spreads to surrounding tissues, progresses towards below the skin, reaches to perianal space, and develops perianal abscess. It progresses upwards through muscles, and develops into supralevator abscess in supralevator space. Or otherwise, it passes horizontally through sphincter muscle, developing into ischiorectal abscess.
As the diagnosis and treatment of anal abscess is delayed, abscess rapidly spreads and becomes more complicated.
Diagnosis of Anal Abscess
Anal examination is sufficient in most cases. In selected cases ultrasound and MR can be required.
What are the treatment methods for anal abscess?
Objective of anal abscess treatment is to correct ano-rectal symptoms and general infection, and to prevent complication of abscess or triggering of other pathologies such as anal fistula.
Abscess drainage is performed under anesthesia. Once the abscess is drained, pain, fever and other symptoms of infection will disappear. Antibiotic, pain management and warm Sitz baths can be used during recovery period.
Patient prescribed with antibiotic treatment after surgical procedure is monitored periodically. Relapse rate is almost 10%. Failure to seek immediate medical assistance, insufficient abscess treatment and abscess location are important determinants in terms of fistula development. Anal fistula develops in 30% of patients with anal abscess.