A fissure in ano is a tear in the anoderm distal to the dentate line. The pathophysiology of anal fissure is thought to be related to trauma from either the passage of hard stool or prolonged diarrhea. A tear in the anoderm causes spasm of the internal anal sphincter, which results in pain, increased tearing, and decreased blood supply to the anoderm. This cycle of pain, spasm, and ischemia contributes to development of a poorly healing wound that becomes a chronic fissure.
The vast majority of anal fissures occur in the posterior midline. 10-15% occur in the anterior midline. Less than 1% of fissures occur off midline.
Symptoms and Signs
Anal fissure is extremely common and characteristic symptoms include tearing pain with defecation, hematochezia (usually described as blood on the toilet paper). Patients also may complain of a sensation of intense and painful anal spasm lasting for several hours after a bowel movement.
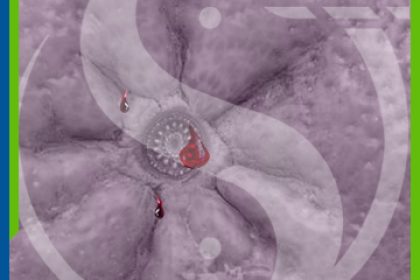
On physical examination, the fissure often can be seen in the anoderm by gently separating the buttocks. Patients are often too tender to tolerate digital rectal examination, anoscopy, or proctoscopy.
An acute fissure is a superficial tear of the distal anoderm and almost always heals with medical management.
Chronic fissures develop ulceration and heaped-up edges with the white fibers of the internal anal sphincter visible at the base of the ulcer.
There often is an associated external skin tag and/or a hypertrophied anal papilla internally. These fissures are more challenging to treat and require surgery. A lateral location of a chronic anal fissure may be evidence of an underlying disease such as Crohn’s disease, HIV, syphilis, tuberculosis, leukemia.
If the diagnosis is in doubt or there is suspicion of another cause for the perianal pain, such as abscess or fistula, an examination under anesthesia may be necessary.
Treatment
Treatment focuses on breaking the cycle of pain, spasm, and ischemia thought responsible for development of fissure in ano.
First-line therapy to minimize anal trauma includes bulk agents, stool softeners, warm Sitz baths. Addition of 2% lidocaine jelly or other analgesic creams can provide additional symptomatic relief. Nitroglycerin ointment (0.2%) has been used locally to improve blood flow but often causes severe headaches. Both oral and topical calcium channel blockers (diltiazem and nifedipine) also have been used to heal fissures and may have fewer side effects than topical nitrates. Newer agents, such as arginine (a nitric oxide donor) and topical bethanechol (a muscarinic agonist), also have been used to treat fissures.
Medical therapy is effective in most acute fissures, and will heal only approximately 50-60% of chronic fissures.
Botulinum toxin (Botox) causes temporary muscle paralysis. Injection of botulinum toxin is used in some centers as an alternative to surgical sphincterotomy for chronic fissure. Although there are few long-term complications from the use of Botox, healing appears to be equivalent to other medical therapies.
Surgical therapy traditionally has been recommended for chronic fissures that have failed medical therapy.
Lateral internal sphincterotomy (LIS) is the procedure of choice for most surgeons. The aim of this procedure is to decrease spasm of the internal sphincter by dividing a portion of the muscle. Approximately 30% of the internal sphincter fibers are divided laterally by using either an open or closed technique. Healing is achieved in more than 95% of patients by using this technique. Most patients experience immediate pain relief. Recurrence occurs in less than 10% of patients. The risk of incontinence (usually to flatus) is 5-15%.